Abstract
INTRODUCTION We have previously observed that many patients with B-cell derived hematologic malignancies fail to produce protective levels of anti-spike antibodies or anti-spike T-cells in response to SARS-CoV-2 mRNA vaccination. We attempted to understand if these results indicated that such patients may be vulnerable to COVID-19 infections.
METHODS The patient-reported LLS National Registry was used to identify patients who had COVID-19 infections including those whose infections occurred after vaccination (breakthrough infections or BTIs) and correlate the BTI with the level of anti-spike antibodies prior to the infection (NCT04806295, NCT04794387). The cohort consisted primarily of patients with chronic lymphocytic leukemia (43%) and other B-cell derived non-Hodgkin lymphomas (35%). Patients self-reported data on demographic variables, vaccine type(s) and dates of administration, date of COVID-19 infection, diagnostic method to detect the infection, and hospitalization date. Anti-spike antibody levels were assessed using the Roche Elecsys semi-quantitative assay. This study was approved by the Western Institutional Review Board, and participants provided informed consent electronically. This survey was conducted on February 17, 2022.
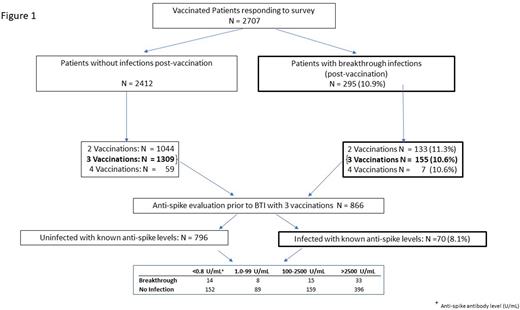
RESULTS 2707 patients who were vaccinated, predominately with SARS-CoV-2 mRNA vaccines, responded to the survey. 295 out of 2707 (10.9%) patients reported BTIs (Figure 1). 80% of BTIs occurred during December 2021 to February 2022, a timing that coincided with the Omicron surge in the general US population. Of the 295 patients who had BTIs, 133/1177 (11.3%), 155/1464 (10.6%), and 7/66 (10.6%) of the patients had 2, 3 or 4 vaccinations, respectively. Among the 866 patients who had three vaccinations and anti-spike antibody analysis, 70 (8.1%) had BTIs. Compared to the population of patients that had three vaccinations who did not develop BTIs, 14/166 (8.2%) and 33/429 (7.6%) patients who had BTIs had undetectable (<0.8 U/mL) or very high levels (>2500 U/mL) of anti-spike antibodies, respectively. There was a moderate association between anti-spike antibody levels and time between 3rd vaccination and BTI (r2 = 0.064, P = 0.03; median values 114 to 138 days for non-detectable and maximum anti-spike levels, respectively). Hospitalizations were reported by 19 of 295 (6.4%) patients. Ten of these patients had anti-spike antibody analysis done after vaccination and prior to the BTI. 100% (10/10) of these patients had anti-spike antibody levels below detectable levels (N = 7) or low anti-spike antibody levels (range : 42-167 U/mL). Nine out of these ten patients had BTIs during the Omicron surge.
CONCLUSIONS AND FUTURE DIRECTIONS
Approximately 10% of patients with hematologic malignancies that had two to four SARS-CoV-2 vaccines reported a BTI during the Omicron surge. The percentage of BTIs was similar regardless of the anti-spike antibody level prior to the infection. In contrast, hospitalization due to a BTI was only found in patients with no detectable anti-spike antibodies or antibody levels previously known to be associated with poor neutralizing antibody levels. Further analysis is on-going to determine if these trends also occur during the BA.5 surge.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal